ICU nursing innovation keeps family connected
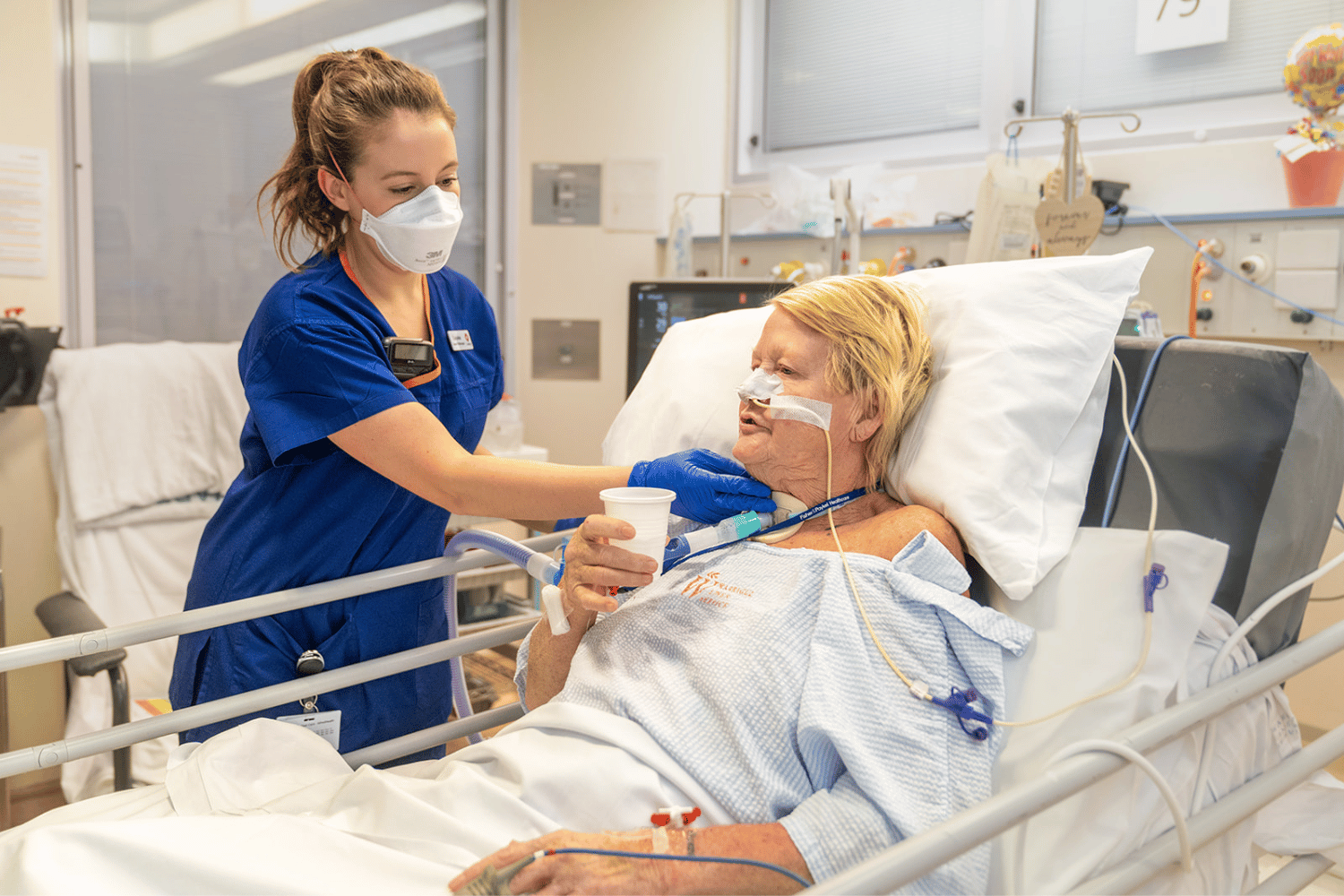
When family and friends were unable to visit The Alfred Hospital during COVID-19, it created new challenges that many of our nurses had not experienced before.
A big challenge for our Intensive Care Unit (ICU) was the loss of the usual face-to-face communication between staff and families.
To help ease an already stressful time for families, an ‘ICU Family Liaison Nurse (FLN) role was created to get information from the ICU unit to families as quickly as possible.
Clinical Nurse Specialist (CNS) Intensive Care Unit, Tanya Brewis, said the aim was to help identify the patient’s primary contact to ensure their family were aware of the various platforms available for communication within the ICU.
“This initiative has now been reviewed and some of the key findings were that the Family Liaison Nurse contacted the majority of families of patients soon after they were admitted to the ICU. During the pandemic, 6536 families were contacted by the FLN, with the average conversation time of 11 minutes, with the maximum call length being two hours,” Tanya said.
In the first 12-months of the role, the FLN also undertook a 72-hour post admission follow-up call with the families, however with increasing ICU bed capacity and subsequent admissions, this workload was not sustainable. However, the FLN was still available to be contacted by families when needed.
While the FLN role has now ended, it has provided a clearer understanding of what is now needed as part of ICU communication.
The initiative, and abstract written by the ICU team, won this year’s Alfred Research Alliance Senior Medical Staff Nursing Research Award for best abstract.
Nursing research, across all disciplines, is critical to improving patient care and we are fortunate to have a strong research program at The Alfred.
